-Prof. Wen-Tsan Chang, General & Digestive Surgery /Director of Transplant Center, Kaohsiung Medical University Chung-Ho Memorial Hospital-
Liver transplantation is widely recognized as one of the most significant breakthroughs in hepatology over the past 30 years. It has proven to be the only effective treatment for patients with acute, fulminant, or chronic liver failure caused by viral hepatitis, alcoholic hepatitis, congenital or acquired metabolic disorders, cholestatic hepatitis, or drug-induced liver injury. Liver transplantation offers better long-term survival rates, quality of life, and return-to-work potential, while also reducing long-term healthcare costs.
Beyond treating liver failure, liver transplantation has now become a key treatment option for liver cancer patients who are not candidates for curative treatments like surgical resection or local ablation, or for those who experience recurrence after such treatments.
From a pathological perspective, liver transplantation is arguably the most ideal treatment for liver cancer. Most liver cancer patients also suffer from liver cirrhosis caused by hepatitis B or C, alcoholic hepatitis, or metabolic disorders such as fatty liver disease, along with complications like jaundice, ascites, and variceal bleeding due to portal hypertension. Liver cancer is also frequently multifocal. As a result, only about 30% of liver cancer patients are suitable candidates for surgical resection or ablation. Furthermore, even after surgery or ablation, the underlying liver cirrhosis remains, which contributes to high recurrence rates — with some studies showing 5-year recurrence rates as high as 70–100%. Therefore, only liver transplantation offers a “root-cause” solution that removes both the tumor and the diseased liver, eliminating the source of recurrence (see Figure 1).
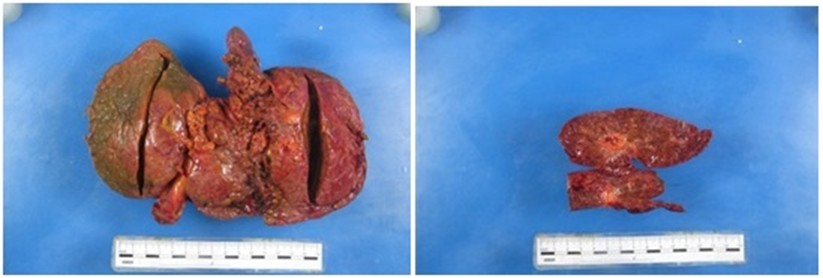
▲Figure 1: Liver removed during transplant shows severe cirrhosis combined with liver cancer.
Although liver transplantation offers significant theoretical and clinical advantages in treating liver cancer, even early-stage patients may have microscopic metastasis to other organs or circulating cancer cells. This explains why approximately 10–15% of patients experience cancer recurrence either in the transplanted liver or elsewhere after transplantation. Reducing post-transplant recurrence has thus become a primary goal of liver transplant teams. Assessing patient eligibility requires evaluating the number, size, and malignancy of the tumors, as well as the presence of vascular invasion or distant metastasis.
The Milan Criteria, accepted by major medical centers worldwide and used by Taiwan’s National Health Insurance for deceased donor liver transplantation, include:
• A single tumor ≤ 5 cm, or
• Up to three tumors, each ≤ 3 cm.
Another widely accepted standard is the UCSF Criteria (University of California, San Francisco), which allow:
• A single tumor ≤ 6.5 cm, or
• Up to three tumors with the largest ≤ 4.5 cm and a total tumor diameter ≤ 8 cm.
The UCSF criteria is also used for Taiwan’s living donor liver transplant coverage.
Patients must not have vascular invasion or distant metastasiswithin both criteria. Those exceeding these criteria must undergo downstaging therapy before being considered for transplantation.
The liver cancer (cirrhosis) treatment team at KMUH brings together experts in hepatobiliary surgery, interventional radiology, and ablation therapy, in collaboration with the hospital’s entire medical staff, to provide comprehensive, high-level multidisciplinary care. In addition, KMUH offers specialized liver transplant outpatient services and an experienced transplant team to support patients who are ineligible for resection or ablation at diagnosis, who have experienced recurrence, or who have end-stage liver cirrhosis.
If you have liver cancer or end-stage liver disease, don’t give up—liver transplantation remains a powerful option. Let’s work together to regain your health and future.
For more articles from KMUH Medical Bulletin, visit:
https://www.kmuh.org.tw/www/kmcj/
All rights reserved. Do not modify the content without permission.
